A Very Public Deception: On the manufacture of mortality statistics in gambling
Part I – Lost in Translation?

In recent years, the claim that up to 496 deaths a year in England are associated with problem gambling has become a staple of the debate on gambling market reform. The estimates originate from a 2023 report by the British Government’s Office for Health Improvement and Disparities (‘OHID’) and have been used to support demands for a wide range of additional controls on consumers and the market. There is just one problem – they are based on junk science.
While it has long been recognised that people with gambling disorder are at elevated risk of self-harm, the specific estimates produced by OHID – accepted uncritically by many in Parliament and the news media – rely on a number of ‘flat-Earth’ assumptions.
In this series of articles, we examine the methods used (and errors made) in calculating these figures and consider the conduct of those who have propagated them. In this, the first article, we demonstrate why the OHID estimates are unsound. In subsequent weeks we will describe the behaviour of the public health officials responsible for their manufacture; consider the actions of other notionally responsible bodies; and ask what public benefit is served by the generation of spurious statistics.
The first state-sponsored estimate of gambling-related suicides in Britain appeared in September 2021 with the release of Public Health England’s (‘PHE’) report, ‘Gambling-related harms evidence review: the economic and social cost of harms’. It contended that, in England, 409 suicides a year were “associated with problem gambling only”. In January 2023, the PHE report was replaced (due to identification of errors) by an update from OHID. It offered a choice of either 117 or 496 suicides “associated with problem gambling”.
Both the PHE and OHID estimates were based on a 2018 study of the medical records of patients treated in Swedish hospitals between 2006 and 2016. Dr Anna Karlsson and Professor Anders Håkansson from Lund University found that patients in the dataset with a clinical diagnosis of ICD-10 ‘pathological gambling’ (renamed gambling disorder in the ICD-11) were on average, 15.1 times more likely to die by suicide compared with the general population. PHE applied suicide mortality ratios from this study to NHS Health Survey estimates of the prevalence of PGSI ‘problem gambling’ in England to produce a figure of 409 deaths a year.
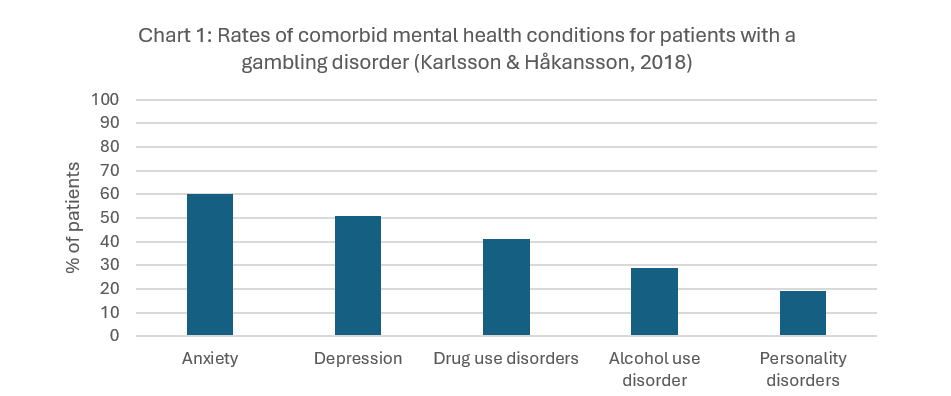
In 2023, OHID repeated the exercise, using precisely the same information, and produced figures of either 117 or 496 deaths (the lower figure based on the application of the Swedish mortality ratios to the population prevalence of DSM-IV ‘pathological gambling’). In doing so they ignored critical information and clear warnings that their methods were unsound. The hospital patients whose records were analysed in the ‘Swedish study’ suffered from a wide range of diagnosed mental and physical health conditions (see charts 1 and 2, below). As a group, they were at elevated risk of self-harm, regardless of the presence or absence of gambling disorder. PHE-OHID thought otherwise - assuming that health risks for hospital patients in Sweden with a wide range of illnesses were the same as for people in England with no diagnosed health disorders whatsoever. In other words, they made the ‘flat-Earth’ assumption that there is no association between mental and physical ill-health and risk of suicide.
In making this assumption, PHE and OHID ignored a clear warning from Karlsson & Håkansson. Their paper advised that the hospital patients whose records they had studied were likely to suffer from particularly severe and complex disorders:
“It is therefore likely that results may be skewed toward a population of individuals with more severe forms of GD [gambling disorder]. It is likely that this once again implies that this study sample might contain patients with higher mental health comorbidity, as well as individuals with more severe forms of GD, since these individuals are more likely to receive specialized psychiatry care”.
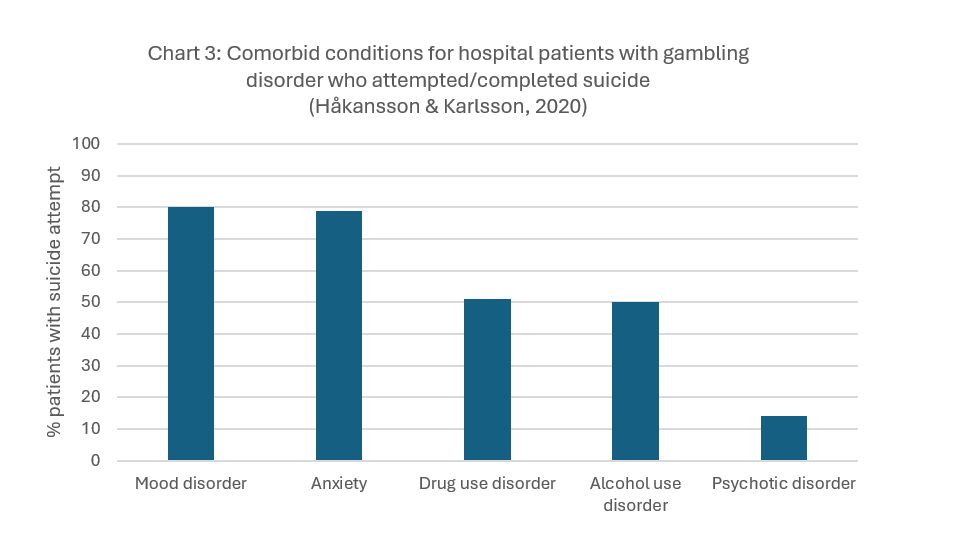
The PHE-OHID researchers also ignored findings from the follow-up to this study (the second in a series of five undertaken by the researchers from Lund University). Håkansson & Karlsson (2020) showed that comorbid health conditions were even higher within the group of patients who had attempted or completed suicide (see chart 3).
Professor Håkansson and Dr Karlsson showed that risk of suicide attempt was five times higher for patients with gambling disorder if they also had diagnoses of alcohol use disorder and drug use disorder. Of those patients who had made a suicide attempt, 70% had a diagnosis of alcohol use disorder or drug use disorder or both. The researchers at Lund University provided a range of adjusted odds ratios based on the presence of other diagnosed mental health conditions (see table 1). This study - which was published ten months prior to the PHE report - indicated that suicide risk for patients with gambling disorder was halved where no alcohol use or drug use disorders were diagnosed. Even before adjusting for other risk factors, these findings clearly demonstrated the inappropriateness of PHE’s approach.
A third study assessed the effect of socioeconomic factors on risk of suicide attempt. In the fourth study, a control group was used to identify discrete risks associated with gambling disorder. It concluded that:
“gambling disorder did not appear to be a significant risk factor for the increase in suicide and general mortality when controlling for previously known risk factors”.
This finding creates a dilemma for OHID and those who have propagated its claims. If one believes that analysis of the Swedish National Patient register by Karlsson & Håkansson provides a reliable basis for assessing suicide risk in England, then one must conclude that – contrary to PHE-OHID assertions – gambling disorder is not “a significant risk factor”. If on the other hand, one does not believe this is a suitable approach, then the PHE-OHID claims also cannot stand because they rely entirely on the mortality ratios from the first of the Swedish studies.
The fact that PHE and OHID got things wrong does not mean that underlying concerns about gambling disorder and self-harm are misplaced – or that gambling operators, treatment providers and policy-makers should ignore the issue. It has long been recognised that people with the disorder are at elevated risk of suicide, even if the precise nature of the relationship is complex. A number of recent inquests in England have determined that excessive gambling contributed to loss of life. Operators should do more to promote positive mental health and to address risk of self-harm among their customers and employees – whether gambling is involved or not. The PHE-OHID claims are, however, irretrievably flawed and should be disregarded by policy-makers. There is simply no coherent logic that allows them to stand.
In next week’s article, we will consider why PHE-OHID produced such obviously flawed findings and examine potentially serious issues of governance attending their publication.
List of abbreviations
DSM-III: The third edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Health Disorders.
DSM-IV: A screening questionnaire published by the American Psychiatric Association within the fourth edition of its Diagnostic and Statistical Manual of Mental Health Disorders
OHID: the Office for Health Improvement and Disparities. Part of the Department of Health and Social Care.
PGSI: The Problem Gambling Severity Index. A screening instrument developed by Ferris & Wynne (2001).
PHE: Public Health England. A state agency, reporting to the Department of Health and Social Care. It was disbanded in 2021.
Dan Waugh is a partner at the global strategic sports and leisure advisory firm, Regulus Partners.